Knee Osteoarthritis: Understanding, Managing, and Treating It
Information reviewed by: Dr. Foo Gen Lin | Last updated: Oct 29, 2025
Knee osteoarthritis causes progressive stiffness and pain that can make staying active challenging. Dr Foo provides proper assessment and personalised treatment to help manage symptoms and maintain your mobility.
MBBS (University of London) | MMed (Ortho) | FRCSEd (Ortho) | FAMS (Ortho)


What Is Osteoarthritis of the Knee?

Knee osteoarthritis (OA) is a degenerative joint condition where the protective
cartilage in the knee joint gradually wears down, leading to pain, stiffness, and
reduced mobility.
It is the most common form of arthritis in the knee and
typically develops over time due to ageing, repetitive stress, or previous injuries. As the
cartilage deteriorates, the bones within the joint begin to rub against each other, causing
inflammation, discomfort, and further joint damage.
In Singapore, knee osteoarthritis is a significant public health concern, affecting an
estimated 4.7% to 11% of adults, with
prevalence increasing sharply after age 40. The condition is more common in women than men
and is more prevalent among Indian and Malay populations compared to Chinese individuals.
With an ageing population and rising obesity rates, the number of people experiencing knee
osteoarthritis is expected to grow.
Causes of Osteoarthritis of the Knees
Knee osteoarthritis develops when cartilage, the smooth, rubber-like tissue that cushions the ends of bones, gradually deteriorates. This loss of protection increases bone friction, leading to bone spur formation and chronic inflammation. The condition is classified into primary and secondary osteoarthritis, based on its cause:
Primary Osteoarthritis
Develops due to natural joint wear over time, often linked to ageing, genetics, and metabolic changes that weaken cartilage and slow its repair.
Secondary Osteoarthritis
Results from external factors or underlying conditions that accelerate joint degeneration, such as previous knee injuries, repetitive high-impact stress, increased joint stress due to excess body weight, and inflammatory diseases like rheumatoid arthritis.
Symptoms of Knee Osteoarthritis
Knee osteoarthritis often develops over several years, with symptoms that may start mildly and intermittently before becoming more persistent and severe. The rate of progression varies, but in most cases, symptoms worsen over time. The most common symptoms include:
- Pain and Swelling – Discomfort arises from inflammation triggered by cartilage breakdown and joint irritation, which can cause excess synovial fluid accumulation (knee effusion), leading to swelling. This swelling, along with increased bone friction, worsens pain during activity but may improve with rest.
- Stiffness and Reduced Motion – Difficulty moving the knee due to joint inflammation, fluid buildup, and narrowing joint space, especially after inactivity.
- Grinding Sensation – A crackling or grating feeling as rough bone surfaces rub together due to cartilage loss.
- Weakness or Instability – A feeling of weakness as damaged cartilage and weakened muscles reduce joint stability, making walking or standing difficult.
Stages of Knee Osteoarthritis
The classification of knee osteoarthritis can be perceived to progress through four stages, determined by the severity of symptoms and the extent of cartilage deterioration.
| Stages | Symptoms |
|---|---|
| Stage 1: Early Degenerative Changes | Minimal cartilage loss, with little or no pain. Small bone spurs may form, but they rarely cause noticeable symptoms. |
| Stage 2: Mild Cartilage Deterioration | Mild pain and stiffness, particularly after prolonged activity or inactivity. Joint space remains mostly intact, though early signs of cartilage thinning may appear. |
| Stage 3: Progressive Cartilage Loss | Significant cartilage loss causes more frequent pain, swelling, and reduced mobility. Joint space narrows, and inflammation becomes more pronounced, making movement increasingly uncomfortable. |
| Stage 4: End-Stage Osteoarthritis | Extensive cartilage loss leads to severe pain, stiffness, and difficulty with daily activities. Bones rub directly against each other, causing chronic inflammation and joint deformity. Surgical intervention, such as knee replacement, is often required to restore function. |
Risk Factors for Knee Osteoarthritis
Knee osteoarthritis often develops due to a combination of mechanical stress and biological factors. Several key risk factors increase the likelihood of developing the condition:
- Ageing – The risk increases with age as cartilage naturally wears down and the body's ability to repair joint tissues declines.
- Gender – Women, especially after menopause, have a higher risk of knee osteoarthritis due to hormonal changes that affect cartilage integrity and joint stability. The decline in estrogen levels may contribute to increased cartilage degradation and osteoarthritis progression.
- Obesity – Excess body weight increases joint stress and promotes inflammation, increasing cartilage breakdown.
- Joint Overuse – Repetitive stress from high-impact activities, sports, or physically demanding jobs contributes to early cartilage deterioration.
- Previous Injuries – Past knee injuries, such as ligament tears or fractures, cause joint instability and inflammation, increasing cartilage wear.
- Genetics – Inherited traits affecting cartilage strength, joint alignment, and inflammatory responses can predispose individuals to osteoarthritis.
- Sedentary Lifestyle – Lack of physical activity weakens muscles that support the knee, reducing joint stability.
Diagnosing Osteoarthritis in the Knee
Diagnosing osteoarthritis involves a combination of physical assessments and imaging tests to evaluate joint condition and severity. These include:
- Medical History – Reviewing the patient's symptoms, lifestyle, medical conditions, and any previous knee injuries to identify potential risk factors.
- Physical Examination – Assessing knee movement, checking for swelling, tenderness, and pain levels, and evaluating joint stability.
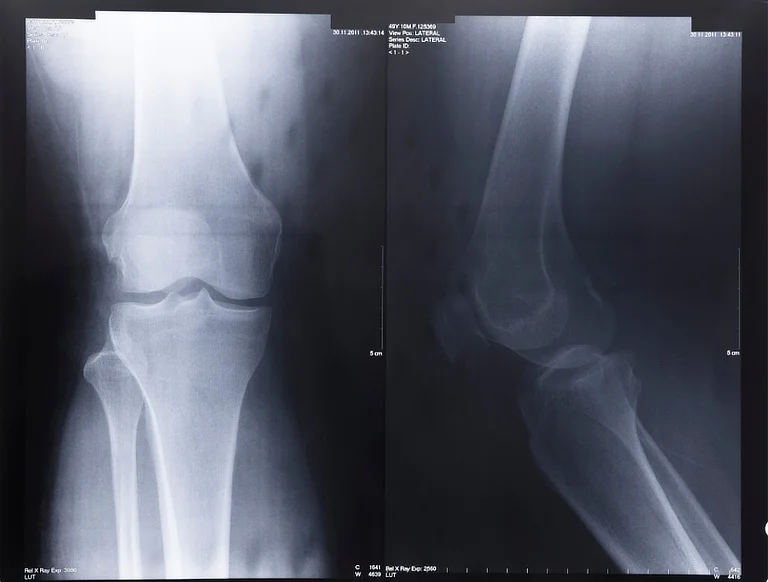
- Imaging Tests – X-rays detect cartilage loss, bone spurs, and joint space narrowing, while MRI scans provide detailed images of soft tissues, helping to identify early cartilage damage and inflammation.
- Joint Fluid Analysis – A sample of synovial fluid is extracted using a needle (arthrocentesis) to check for infection, inflammation, or conditions like gout that may mimic osteoarthritis symptoms.
Early diagnosis is essential for managing knee osteoarthritis, as it helps determine the severity of cartilage damage and guides treatment.
How to Treat Osteoarthritis in the Knee?
While knee osteoarthritis cannot be reversed, treatment typically involves a combination of approaches to manage symptoms, improve mobility, and slow disease progression.
| Treatment | Description |
|---|---|
| Non-Surgical Management | |
| Swelling & Pain Management | Medications like paracetamol or NSAIDs (e.g., ibuprofen) help control pain and inflammation. Topical treatments, such as capsaicin or menthol creams, provide targeted relief. |
| Supportive Devices | Knee braces provide stability, while orthotic insoles distribute weight evenly. Walking aids, such as canes or walkers, help offload pressure, and compression sleeves may reduce swelling. Shock-absorbing footwear minimises joint impact for added comfort. |
| Lifestyle Modification | Making lifestyle changes, such as managing weight to reduce stress on the knee joint and avoiding activities that worsen symptoms, can help slow cartilage deterioration. |
| Physical Therapy & Exercise | Exercises designed to strengthen the muscles around the knee improve joint stability and mobility while reducing pain and stiffness. |
| Injection-Based Treatment | Corticosteroid injections temporarily reduce inflammation and pain. Hyaluronic acid injections can help to improve joint lubrication, reducing friction and stiffness. Platelet-Rich Plasma (PRP) therapy may also promote tissue healing and reduce inflammation. |
| Surgical Intervention | |
| Arthroscopy | A minimally invasive procedure to remove damaged cartilage or smooth rough joint surfaces, reducing pain and improving movement. |
| Osteotomy | A bone realignment surgery that redistributes weight away from the damaged area, relieving pressure on the affected knee and potentially delaying the need for joint replacement. |
| Partial or Total Knee Replacement | Knee replacement surgery restores function and relieves pain by replacing damaged joint surfaces with prosthetic implants. Partial knee replacement preserves healthy tissue by replacing only the affected area, while total knee replacement replaces the entire joint, typically for severe osteoarthritis. |
How to Prevent Knee Osteoarthritis?
While some risk factors like ageing and genetics cannot be controlled, you can take steps to reduce your risk:

- Maintain a Healthy Weight – Reduces stress on the knee joints and slows cartilage wear.
- Stay Active – Regular exercise strengthens muscles, improves joint stability, and supports overall knee health.
- Protect Your Knees – Avoid excessive impact activities and use proper techniques during sports and exercise.
- Eat a Balanced Diet – Nutrient-rich foods, including omega-3 fatty acids, calcium, and vitamin D, help maintain strong bones and cartilage.
- Manage Injuries Early – Prompt treatment of knee injuries prevents long-term joint damage and reduces the risk of osteoarthritis.
Summary
Knee osteoarthritis is a progressive condition that can significantly affect your mobility
and quality of life, but various treatments can help manage symptoms and improve joint
function.
While it cannot be reversed, options such as lifestyle modifications, physical therapy,
pain management, and, if necessary, surgery can relieve discomfort and enhance movement. Prompt
diagnosis and treatment are key to slowing the progression of the condition.
If you experience persistent knee pain or stiffness, consider seeking
medical advice early as it can lead to better management and improved long-term joint
health.
Managing your knee osteoarthritis is about finding the right balance of treatment to maintain your quality of life. Options range from lifestyle modifications and injections to surgical intervention when needed.
Where Can I Find a Knee Specialist in Singapore?
Apex Novena
admin@apexsportsclinic.sg
101 Irrawaddy Rd, #18-12 Royal Square Medical Centre, Singapore 329565
Nearest MRT: NS20 Novena (3-min walk)
Wheelchair Accessible
Apex East Coast
admin@apexsportsclinic.sg
112 East Coast Rd, #03-03/04 i12 Katong, Singapore 428802
Nearest MRT: TE26 Marine Parade (7-min walk)
Wheelchair Accessible
Why Do Patients Choose Apex Sports Clinic?
Sports Doctor in Singapore: Personalised & Affordable Care
Progressive Treatment Philosophy
We prioritise personalised, non-invasive solutions, progressing to specialised treatments, including surgery, only when needed for more effective and targeted care.
Holistic Patient-Centred Care
From diagnosis to rehabilitation, we provide comprehensive and seamless care for a wide range of orthopaedic conditions.
Specialist in Sports Orthopaedics & Injury Management
We combine expert injury management with a proactive approach to maintaining your body's strength and function, so you can recover fully and perform at your peak.
Patient Journey
1 . Schedule Your Appointment

2 . Expert Diagnosis & Consultation

3 . Customised Treatment Plan

Schedule an Appointment

Our Insurance Partners








Frequently Asked Questions (FAQs)
There is no single solution for knee osteoarthritis, but a range of treatment options is available to manage the condition based on its severity. Non-surgical treatments include lifestyle modifications, physical therapy, weight management, pain-relief medications, and joint injections. For advanced cases, surgical options such as knee arthroscopy, osteotomy, or knee replacement surgery may be recommended. It is best to consult an orthopaedic specialist for a proper evaluation and treatment plan for your condition.
Knee osteoarthritis is caused by the gradual breakdown of cartilage that cushions the knee joint. This degeneration leads to bone friction, inflammation, and joint pain. Ageing is the primary cause, but factors like past injuries, genetics, obesity, repetitive stress, and metabolic changes also contribute. Secondary osteoarthritis can result from inflammatory conditions or joint misalignment.
A knee brace can provide additional support, improve stability, and help reduce pain by offloading pressure from affected areas of the joint. While it does not reverse osteoarthritis, it can aid mobility and enhance comfort during daily activities. The effectiveness of a knee brace depends on the severity of the condition and the type of brace used. It is advisable to consult a doctor to determine if a knee brace is suitable for your condition.
Gentle stretching can improve flexibility and reduce stiffness in knee osteoarthritis. Effective stretches include quadriceps, hamstring, calf, and seated knee extensions, which help maintain mobility and support joint function. It is best to consult a doctor or physiotherapist for personalised exercises and guidance to prevent strain and promote proper movement.
Preventing further osteoarthritis progression after knee surgery involves regular follow-ups with your doctor or physiotherapist, maintaining a healthy weight, engaging in low-impact exercises, strengthening the muscles around the knee, and following a structured rehabilitation programme. Protecting the knee from excessive stress and using proper movement techniques can also help reduce the risk of joint deterioration.
Strengthening exercises for the quadriceps, hamstrings, and calf muscles can help support the knee and reduce cartilage stress. Low-impact activities like leg lifts, straight-leg raises, seated knee extensions, and resistance band exercises help to improve stability and function. It is best to consult your doctor or physiotherapist to ensure the exercises suit your condition and are done correctly.
Currently, there is no cure for knee osteoarthritis, but various treatments can help manage symptoms and slow the disease's progression. Lifestyle changes, physical therapy, medication, and in some cases, surgery, can help improve joint function and reduce pain. Early intervention and consistent management strategies are key to maintaining mobility and quality of life.
Therapy for knee osteoarthritis typically involves physiotherapy, pain management, and lifestyle modifications. Physiotherapy strengthens the muscles around the knee, improves flexibility, and enhances joint stability. Pain relief methods may include medications, heat or cold therapy, and joint injections. It is best to consult a doctor or orthopaedic specialist for a treatment plan tailored to your needs.
Yes, a knee brace can help manage knee osteoarthritis by providing support, reducing pain, and improving stability. It can be particularly useful for individuals with mild to moderate osteoarthritis or joint misalignment. However, a knee brace should be part of a comprehensive treatment plan rather than a standalone solution. It is best to consult your doctor or orthopaedic specialist to determine the most suitable brace for your condition.
Diagnosing knee osteoarthritis involves a combination of physical examinations and imaging tests. Special tests include X-rays to detect cartilage loss, bone spurs, and joint space narrowing, while MRI scans may be used to evaluate soft tissue damage. In some cases, joint fluid analysis (arthrocentesis) is performed to rule out other conditions like gout or infection. It is best to consult a doctor or orthopaedic specialist for a thorough assessment of your condition.
The best treatment for knee osteoarthritis depends on its severity. Early-stage cases may be managed with weight management, physical therapy, and pain relief medications. Moderate cases may benefit from joint injections like corticosteroids or hyaluronic acid for temporary relief. Severe osteoarthritis may require surgical options such as knee replacement to restore function and reduce pain. It is best to consult a doctor or orthopaedic specialist for a treatment plan suited to your needs.
Massage therapy may provide temporary relief by improving circulation, reducing muscle tension, and alleviating stiffness around the knee joint. However, it does not treat the underlying cause of osteoarthritis. Gentle massage, when combined with other treatments such as exercise and physiotherapy, may help improve overall joint function and comfort. It is best to consult your doctor or specialist for personalised advice on whether massage is suitable for your condition.
A normal knee has a smooth cartilage layer that cushions the joint, allowing for pain-free movement. In contrast, an osteoarthritis knee experiences cartilage breakdown, leading to joint space narrowing, increased bone friction, inflammation, and pain. Over time, the knee may develop bone spurs, stiffness, and deformity, affecting mobility.
Secondary osteoarthritis develops due to underlying factors that accelerate joint degeneration. Common causes include previous knee injuries (e.g., ligament tears or fractures), obesity, inflammatory conditions such as rheumatoid arthritis, metabolic disorders like diabetes, and repetitive joint stress from certain occupations or sports.
Treatment for knee osteoarthritis includes lifestyle changes, physical therapy, medication, and, in severe cases, surgery. Weight management, low-impact exercises, and knee braces can help reduce joint strain. Pain relief options include NSAIDs, corticosteroid injections, and hyaluronic acid injections. Surgery, such as knee replacement, may be considered if other treatments fail. It is best to consult a doctor or orthopaedic specialist for the most appropriate treatment for your condition.
Osteoarthritis knee pain is typically a dull, aching discomfort that worsens with movement and improves with rest. It may be accompanied by stiffness, swelling, and a grinding sensation in the joint. Some individuals experience sharp pain during weight-bearing activities or after prolonged periods of inactivity.
Yes, walking is generally beneficial for knee osteoarthritis as it helps maintain joint mobility and strengthen surrounding muscles. However, it is important to walk on even surfaces, wear supportive footwear, and pace activity to avoid excessive strain. If walking worsens pain, reducing intensity or switching to low-impact exercises like swimming may be advisable. It is best to consult your orthopaedic specialist or physiotherapist to determine if walking is suitable for your condition.
While osteoarthritis cannot be completely stopped, its progression can be slowed with proper management. Maintaining a healthy weight, staying active, and avoiding excessive joint stress can help preserve knee function and delay further cartilage loss. Treatment options such as physical therapy, medications, and joint injections may also help manage symptoms and improve mobility. It is best to consult a doctor or orthopaedic specialist to determine the most appropriate treatment approach for your condition.
Individuals with knee osteoarthritis should avoid high-impact activities such as running or jumping, prolonged periods of inactivity, and excessive weight gain, as these can worsen joint strain. Poor posture, improper exercise techniques, and excessive kneeling or squatting may also exacerbate symptoms. It is best to consult a doctor or orthopaedic specialist for personalised lifestyle advice and activity modifications suited to your condition.
There is no definitive list of foods that worsen knee osteoarthritis, but processed foods, refined sugars, excessive salt, and trans fats may increase inflammation and joint discomfort. Red and processed meats, fried foods, and sugary beverages have been linked to higher inflammatory markers. It is best to consult a doctor or nutritionist for dietary advice tailored to your condition.
No, knee osteoarthritis is a chronic condition that does not go away, but symptoms can be managed with treatments such as physical therapy, weight management, pain relief medications, and joint injections. In severe cases, surgical options like knee replacement may be considered. It is best to consult a doctor or orthopaedic specialist for the most appropriate treatment approach for your condition.
Drinks with anti-inflammatory properties, such as green tea, turmeric milk, and tart cherry juice, may help manage joint inflammation. Staying hydrated with plain water is also important for joint health. It is best to consult a doctor or nutritionist for dietary advice suited to your condition.
Mild knee pain can improve with movement, as walking helps maintain joint function and reduces stiffness. However, if pain is severe, short rest periods combined with gentle movement may be necessary to prevent overexertion. It is best to consult your doctor or physiotherapist for personalised advice on managing mobility.
Prolonged sitting can contribute to joint stiffness and reduced circulation, potentially worsening osteoarthritis symptoms. Regular movement and stretching throughout the day can help maintain joint flexibility. It is advisable to consult your doctor or physiotherapist for personalised guidance on managing activity levels.
Walking may still be possible in stage 4 osteoarthritis, but it can be challenging due to severe pain and joint stiffness. Walking aids, knee braces, and low-impact movement strategies can help manage mobility. It is best to consult a physiotherapist or orthopaedic specialist for personalised advice on movement and treatment options.
Most individuals with osteoarthritis do not require a wheelchair if managed with treatments like physical therapy, weight management, pain relief medications, joint injections, and knee braces. Severe cases may require surgical options such as knee replacement. It is best to consult a doctor or orthopaedic specialist for the most suitable treatment for your condition.
Vitamin E has antioxidant properties that may help reduce inflammation, but there is limited scientific evidence supporting its effectiveness in directly treating osteoarthritis. Other nutrients, such as omega-3 fatty acids, calcium, and vitamin D, play a more established role in supporting joint health and reducing inflammation. It is best to consult your doctor or a nutritionist for guidance on supplements and dietary choices suited to your condition.

