Dislocated Shoulder: Treatment for First-Time and Recurrent Injuries
Information reviewed by: Dr. Foo Gen Lin | Last updated: Oct 29, 2025
Experiencing shoulder instability after an injury or fall? Dr Foo provides prompt evaluation and personalised care to restore stability and help prevent future dislocations.
MBBS (University of London) | MMed (Ortho) | FRCSEd (Ortho) | FAMS (Ortho)


What Is a Dislocated Shoulder?
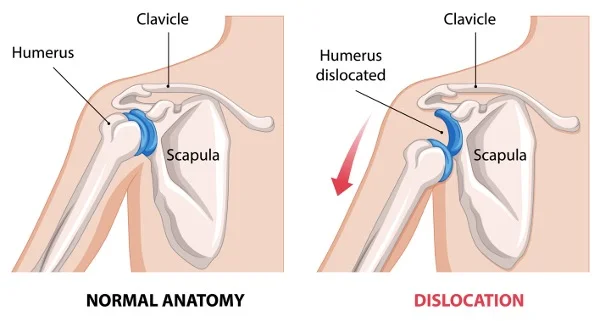
A dislocated shoulder occurs when the upper arm bone (humerus) moves out of its
normal position in the shoulder joint. This injury commonly results from falls,
sports injuries, or direct trauma, and can lead to significant pain, instability, and
reduced mobility.
Seeking prompt medical evaluation and treatment is essential to restore shoulder function
and prevent further complications, such as recurrent dislocations, nerve damage, or
long-term joint instability.
Types of Shoulder Dislocations
There are three primary types of shoulder dislocations (anterior, posterior, and inferior) depending on how the humerus shifts out of position:
1. Anterior Shoulder Dislocation
An anterior dislocation occurs when the humerus moves forward out of the joint. It is the most common type, accounting for the majority of shoulder dislocation cases. This type of dislocation is often caused by falls, sports injuries, or direct impact.
2. Posterior Shoulder Dislocation
A posterior dislocation occurs when the humerus shifts backward. It is less common and can result from seizures, electric shocks, or falls on an outstretched arm.
3. Inferior Shoulder Dislocation
An inferior dislocation occurs when the humerus moves downward. It is the least frequent type of shoulder dislocation and is usually associated with high-force trauma. In some cases, it may also involve nerve or blood vessel injury.
Causes of Shoulder Dislocation
A shoulder dislocation typically occurs due to a sudden force or trauma that overwhelms the joint’s supporting tissues. Common causes include:

- Sports Injuries – Contact sports such as rugby, football, and martial arts increase the risk of shoulder dislocation due to high-impact collisions and falls.
- Falls – Landing on an outstretched arm or directly on the shoulder can force the joint out of place.
- Accidents – High-impact incidents, such as motor vehicle collisions or workplace injuries, can generate enough force to dislocate the shoulder.
- Repetitive Overhead Motions – Activities like swimming, baseball, or weightlifting can gradually alter shoulder mechanics by straining ligaments, weakening muscles, and changing joint stability.
Dislocated Shoulder Symptoms
A dislocated shoulder presents with clear and immediate symptoms at the point of injury, including:
- Sudden onset of severe pain, often worsening with movement.
- Visible deformity, where the shoulder may appear misaligned or squared off.
- Limited or complete loss of movement, where the affected arm may be difficult or impossible to move.
- Swelling and bruising, caused by the body's inflammatory response to injury as blood vessels rupture and fluid accumulates in the surrounding tissues.
- Numbness or tingling, due to nerve involvement, which may cause altered sensation in the arm.
Diagnosing a Dislocated Shoulder
Diagnosing a dislocated shoulder typically involves a physical examination and, if necessary, imaging tests:

- Medical History Review – Assesses previous shoulder injuries, underlying joint conditions, and the circumstances leading to the dislocation to identify risk factors and potential complications.
- Physical Examination – Evaluates shoulder position, range of motion, and neurological function by assessing pain levels, muscle strength, and any signs of nerve involvement.
- X-rays – Confirms the dislocation and rules out fractures or other bone abnormalities that may require additional treatment.
- MRI or CT scans – Provides a detailed view of soft tissue structures, helping to identify ligament tears, cartilage damage, or other injuries that may contribute to joint instability.
Shoulder Dislocation Treatment & Management
Treatment for a dislocated shoulder depends on the severity, type of dislocation, and associated
injuries.
Initial management typically begins with pain relief, reduction of the dislocation,
immobilisation, followed by rehabilitation. Surgical intervention may be required in cases of
recurrent dislocation, failure of non-surgical treatment to restore stability, or significant
structural damage to the shoulder joint.
| Treatment | Description & Purpose |
|---|---|
| Non-Surgical Management | |
| Immobilisation and Rest | The arm is kept still in a sling or splint to prevent further movement and support initial healing. This helps reduce pain, minimise swelling, and lower the risk of additional damage to the joint and surrounding tissues. |
| Pain Management | Medications such as non-steroidal anti-inflammatory drugs (NSAIDs) or local anaesthetics help manage pain and inflammation, ensuring comfort and aiding recovery. Applying ice packs for the first 48 hours can help reduce swelling and numb pain. Pain relief can also facilitate closed reduction by relaxing muscles and minimising resistance during shoulder realignment. |
| Closed Reduction | Manual manipulation of the shoulder to realign the joint and restore function without surgery. It is typically performed as part of immediate management following the injury. |
| Physiotherapy | Rehabilitation exercises begin after initial healing following closed reduction, focusing on gradually strengthening the shoulder muscles and improving joint stability to restore function and reduce the risk of future dislocations. |
| Surgical Intervention | |
| Arthroscopic Stabilisation | A minimally invasive surgical procedure that repairs torn ligaments and reinforces the shoulder joint, reducing the likelihood of recurrent dislocations. |
| Latarjet Procedure | A surgical technique that involves transferring a small piece of bone from the coracoid process (a bony projection on the front of the shoulder blade) to the front of the shoulder socket to strengthen the joint and prevent future dislocations. It is typically performed for recurrent shoulder dislocations, especially when there is bone loss in the shoulder socket. |
| Open Reduction and Internal Fixation (ORIF) | A surgical procedure in which fractured bones in the shoulder are stabilised using screws or plates to ensure proper healing and restore joint function. It is typically performed when a shoulder dislocation is accompanied by fractures of the ball of the upper arm bone or the shoulder socket. |
Dislocated Shoulder Recovery

Recovery time varies depending on the severity of the injury, treatment approach, and individual healing process. Typical recovery timelines include:
- Mild dislocation – 2 to 6 weeks for initial healing, with the arm typically immobilised in a sling for 1 to 3 weeks. Physiotherapy can help restore movement and prevent stiffness.
- Severe dislocation or surgery – 3 to 6 months before returning to full activity, with a longer period of immobilisation followed by structured rehabilitation.
- Return to sports – 4 to 6 months, depending on strength, joint stability, and sport-specific demands.
Preventing Shoulder Dislocations
Preventative measures can help reduce the risk of future dislocations, especially for individuals with prior injuries or joint instability:
- Strengthening Shoulder Muscles – Targeted exercises for the rotator cuff, deltoid, and scapular stabilisers can enhance joint support and stability, reducing the likelihood of dislocations.
- Improving Flexibility – Regular stretching maintains joint mobility and balance, preventing stiffness and excessive strain on ligaments and muscles.
- Using Protective Gear – Shoulder braces or padding help stabilise the joint and absorb impact, particularly in contact sports or high-risk activities.
- Practising Proper Techniques – Correct movement patterns, proprioceptive training, and neuromuscular control exercises minimise undue stress on the shoulder, lowering the risk of recurrent dislocations.
When to Seek Medical Attention
Seek medical attention if you suspect a dislocated shoulder or if you experience:
- Persistent shoulder pain or instability that does not improve.
- Weakness, numbness, or tingling in the arm, which may suggest nerve involvement.
- Limited shoulder movement that affects daily activities, such as dressing, lifting, or reaching.
If you have experienced repeated shoulder dislocations despite preventive measures, consider consulting a shoulder specialist for a more targeted treatment approach.
A dislocated shoulder requires proper assessment to check for associated injuries. Whether it is your first dislocation or a recurring issue, we will work with you to find the right approach for your situation.
Find a Shoulder Specialist Near Me
Apex Novena
admin@apexsportsclinic.sg
101 Irrawaddy Rd, #18-12 Royal Square Medical Centre, Singapore 329565
Nearest MRT: NS20 Novena (3-min walk)
Wheelchair Accessible
Apex East Coast
admin@apexsportsclinic.sg
112 East Coast Rd, #03-03/04 i12 Katong, Singapore 428802
Nearest MRT: TE26 Marine Parade (7-min walk)
Wheelchair Accessible
Why Do Patients Choose Apex Sports Clinic?
Sports Doctor in Singapore: Personalised & Affordable Care
Progressive Treatment Philosophy
We prioritise personalised, non-invasive solutions, progressing to specialised treatments, including surgery, only when needed for more effective and targeted care.
Holistic Patient-Centred Care
From diagnosis to rehabilitation, we provide comprehensive and seamless care for a wide range of orthopaedic conditions.
Specialist in Sports Orthopaedics & Injury Management
We combine expert injury management with a proactive approach to maintaining your body's strength and function, so you can recover fully and perform at your peak.
Patient Journey
1 . Schedule Your Appointment

2 . Expert Diagnosis & Consultation

3 . Customised Treatment Plan

Schedule an Appointment

Our Insurance Partners








Frequently Asked Questions (FAQs)
The most common type of shoulder dislocation is anterior dislocation, where the upper arm bone (humerus) moves forward out of the shoulder socket. It accounts for the majority of shoulder dislocation cases and typically occurs due to falls, sports injuries, or direct impact. This type of dislocation often affects active individuals and contact sport athletes because of the high stress placed on the shoulder joint.
Recurrent shoulder dislocation is relatively common, particularly among younger and more active individuals. The risk depends on factors such as age, activity level, and the extent of ligament or bone injury during the initial episode. Without proper rehabilitation and preventive measures, the shoulder may remain unstable and prone to re-injury. You should always follow your doctor’s or shoulder specialist’s guidance on preventing future dislocations.
Rehabilitation after a shoulder dislocation focuses on restoring movement, strength, and stability. Common exercises include gentle range-of-motion stretches, rotator cuff and scapular stabilisation exercises, and progressive resistance training as healing progresses. These help rebuild muscle support and improve joint control, reducing the risk of recurrence. It is advisable to follow your physiotherapist’s or specialist’s recommended rehabilitation programme to support a smooth recovery.
The fastest recovery from a dislocated shoulder involves early medical treatment, followed by immobilisation, gradual physiotherapy, and muscle strengthening. Prompt reduction of the dislocation and adherence to a structured rehabilitation plan help restore mobility while preventing re-injury. While healing speed varies with injury severity, avoiding premature return to activity supports long-term stability and recovery. Always follow the advice of your specialist or physiotherapist during treatment.
Driving is generally not advisable immediately after a shoulder dislocation, as pain, stiffness, and limited movement can affect control and reaction time. Most individuals are advised to wait until the shoulder has regained sufficient strength and range of motion, which typically occurs after the sling is discontinued and early rehabilitation is completed. Always follow the advice of your doctor or specialist before resuming driving.
Persistent shoulder pain after treatment can be normal during early recovery but may also indicate incomplete healing, soft tissue injury, or nerve irritation. Mild discomfort usually improves with rest and physiotherapy, but ongoing or worsening pain should be evaluated to rule out complications such as recurrent instability or labral tears. If your shoulder continues to hurt significantly, it is advisable to consult your orthopaedic specialist.
The most comfortable sleeping position after a shoulder dislocation is typically lying on your back with a pillow supporting the injured arm or upper body. This helps keep the shoulder in a neutral position and reduces strain. Side sleeping on the uninjured arm with the affected arm supported by a cushion is another option once pain decreases. Always follow your specialist’s or physiotherapist’s recommendations for sleeping posture during recovery.
Healing time for a dislocated shoulder varies depending on injury severity and treatment. Mild cases may recover within 2 to 6 weeks, while more severe dislocations or those requiring surgery may take 3 to 6 months. Rehabilitation is essential to restore full strength and stability and to prevent recurrence. Returning to sports or strenuous activities too early can delay healing or cause re-injury. It is best to consult your doctor or specialist on your expected recovery timeline.
A dislocated shoulder is treated through a procedure called closed reduction, in which a doctor carefully repositions the joint. This is usually followed by immobilisation in a sling to support healing, then physiotherapy to restore strength, flexibility, and stability. In recurrent or complex cases, surgical options such as arthroscopic stabilisation or the Latarjet procedure may be required. If you suspect a dislocated shoulder, it is advisable to seek prompt medical attention.
A dislocated shoulder typically causes sudden, intense pain, visible deformity, and an inability to move the arm. The shoulder may appear squared or out of place, and swelling, bruising, or numbness in the arm or hand can occur due to nerve involvement. Some people describe a sensation of the shoulder “popping out.” If you experience these symptoms, it is advisable to seek prompt medical attention.
After recovery, some individuals may experience lingering shoulder weakness, stiffness, or reduced range of motion. Recurrent dislocations or chronic instability can develop if ligaments or soft tissues fail to heal properly. In some cases, early joint wear (arthritis) may occur over time. Comprehensive rehabilitation and adherence to strengthening exercises can greatly reduce these long-term risks
If your shoulder dislocates, avoid moving or forcefully rotating the arm, lifting heavy objects, or engaging in strenuous activity until cleared by a doctor. Premature movement may worsen the injury or cause re-dislocation. It is also important not to attempt self-reduction, as improper handling can damage nerves or blood vessels. You should seek immediate medical attention to ensure the joint is properly realigned and treated.
A sling is typically worn for one to three weeks after a mild shoulder dislocation to allow tissues to heal and reduce pain. More severe injuries or those treated surgically may require immobilisation for up to six weeks. The duration depends on the type of dislocation, patient age, and healing progress. Always follow your specialist’s or physiotherapist’s guidance before discontinuing the sling or resuming activity.
A dislocated shoulder cannot realign or fully heal on its own and requires medical intervention to reposition the joint safely. Without proper reduction and rehabilitation, the shoulder may remain unstable or suffer long-term complications. Early treatment ensures proper healing of ligaments and reduces the risk of recurrent dislocations. If you suspect a shoulder dislocation, it is advisable to seek immediate medical care.
Movement is usually severely restricted after a shoulder dislocation due to intense pain, muscle spasms, and joint misalignment. Some limited movement of the hand or wrist may still be possible, but raising or rotating the arm is often impossible. Forcing movement can worsen tissue damage or affect nerves and blood vessels. If you suspect a dislocation, immobilise the arm and seek urgent medical attention.
Shoulder fractures, rotator cuff tears, and severe sprains can sometimes be mistaken for a dislocated shoulder because they share symptoms such as pain, swelling, and restricted motion. However, a dislocation typically causes visible deformity or an abnormal shoulder contour. Imaging such as X-rays or MRI scans is essential for proper diagnosis and appropriate treatment.
A shoulder dislocation is considered a significant injury because it involves the displacement of a major joint and potential damage to ligaments, tendons, or nerves. While many cases recover with proper treatment and rehabilitation, repeated dislocations or untreated injuries can lead to chronic instability or arthritis. Prompt management by a doctor or specialist helps reduce the risk of long-term complications.
A single shoulder dislocation usually heals without lasting damage if treated promptly and followed by proper rehabilitation. However, repeated dislocations or severe trauma can stretch or tear ligaments, leading to chronic instability or cartilage wear over time. In some cases, this may contribute to early joint degeneration or arthritis. If you experience persistent weakness or instability, it is advisable to consult a shoulder specialist.

