Knee Meniscus Tear & Injury: Causes, Symptoms & Treatment
Information reviewed by: Dr. Foo Gen Lin | Last updated: Oct 29, 2025
Knee meniscus tears can cause pain, instability, and reduced mobility if left untreated. Dr Foo offers detailed evaluation and tailored care to restore function and support long-term knee health.
MBBS (University of London) | MMed (Ortho) | FRCSEd (Ortho) | FAMS (Ortho)


What Is the Knee Meniscus?
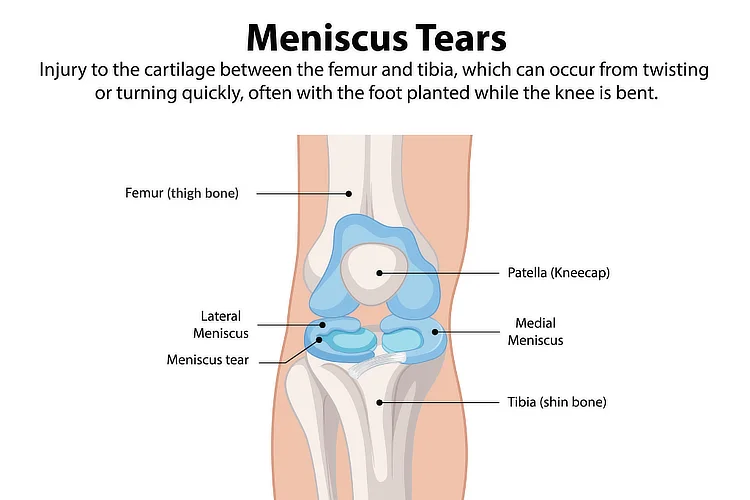
The knee meniscus is a C-shaped piece of fibrocartilage located between the
thighbone (femur) and the shinbone (tibia) in each knee joint.
Each knee has two menisci, with the medial meniscus on the inner side and
the lateral meniscus on the outer side. They act as shock absorbers,
cushioning the joint and distributing weight evenly during movement.
The menisci play a crucial role in stabilising the knee, reducing
friction,
and protecting the cartilage from wear and tear. When strained or damaged,
they can cause
pain, swelling, and restricted movement.
If left untreated, a meniscus injury may lead to long-term joint problems, including osteoarthritis.
Types of Meniscus Injuries
There are several types of meniscus injuries, each affecting the knee joint differently depending on the nature and extent of the damage.
| Type of Injury | Description |
|---|---|
| Meniscus Tear | Tears can affect either the medial or lateral meniscus. Common types include radial, horizontal, flap, bucket-handle, and degenerative tears. |
| Meniscus Degeneration | Degenerative changes occur due to ageing and repetitive stress, making the meniscus more prone to tears. |
| Meniscal Cysts | A fluid-filled sac caused by chronic irritation or past tears. Large cysts may lead to swelling and restricted movement. |
| Meniscal Extrusion | Meniscal extrusion occurs when the meniscus moves out of place due to trauma or degeneration. It is often associated with osteoarthritis and cartilage wear. |
| Meniscal Calcification (Chondrocalcinosis) | Calcium deposits form in the meniscus, often linked to joint conditions like pseudogout, resulting in stiffness and discomfort. |
Symptoms of a Meniscus Tear

A torn meniscus can cause pain, discomfort, and restricted movement, with symptoms varying based on the severity and location of the tear.
- A popping sensation at the time of injury.
- Knee pain that worsens with movement or weight-bearing.
- Swelling that develops over a few hours to days, often due to knee effusion, as excess synovial fluid accumulates in response to the injury.
- Difficulty fully extending or bending the knee.
- A sensation of the knee locking or catching.
- Instability when walking or bearing weight.
If left untreated, a meniscus tear can lead to chronic knee pain, persistent swelling, joint stiffness, and increased risk of osteoarthritis.
Meniscus Tear Grades
Meniscus tears can be classified based on severity and depth, which influence symptoms and knee function.
- Grade 1 (Mild) – Small tears in the outer layer of the meniscus, often asymptomatic or causing slight discomfort.
- Grade 2 (Moderate) – Partial tears extend deeper into the meniscus, causing pain, swelling, and occasional knee catching.
- Grade 3 (Severe) – Full-thickness tears through the entire meniscus, leading to knee locking, instability, and significant pain.
Meniscus Tear Causes
Meniscus tears can occur due to excessive twisting, direct trauma, or long-term degeneration of the knee.
- Sudden pivoting or twisting during sports like football, basketball, and tennis, increasing the risk of acute tears.
- Direct blows or forceful impact to the knee in contact sports like rugby or football, which can compress or shear the meniscus, leading to a tear.
- Improper squatting or lifting heavy objects, placing excessive strain on the meniscus and surrounding knee structures.
- Age-related degeneration, which weakens the meniscus over time, making it more susceptible to tearing.
- Discoid meniscus, a congenital abnormality that increases instability and tear risk.
How to Diagnose a Meniscus Tear?
Diagnosing a meniscus tear involves a combination of clinical assessment and imaging to determine the severity and location of the injury.
1. Physical Examination
A visual and manual examination to evaluate knee movement, joint stability, and pain response.
2. McMurray Test
A test involving bending, rotating, and straightening the knee to detect pain, clicking, or locking, which may indicate a meniscus tear.
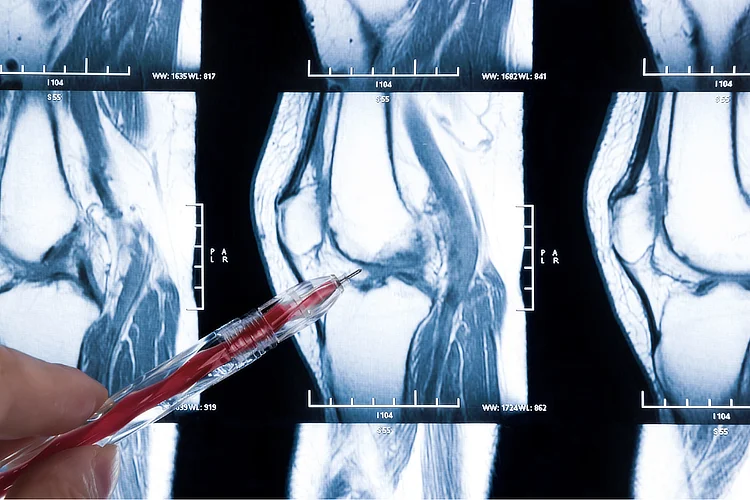
3. Imaging Tests
- X-rays – Typically the first imaging tool used to rule out fractures or other bone-related issues.
- Magnetic Resonance Imaging (MRI) – Provides detailed images of knee structures to confirm the location and extent of the tear.
- Ultrasound – May be used in specific cases to assess soft tissue injuries affecting the meniscus.
Meniscus Tear Treatment
Treatment for meniscus tears depends on the severity, location of the tear, age,
and activity level. Management often involves a combination of approaches.
Non-surgical options are typically recommended for mild to moderate tears, while surgical
intervention may be necessary for severe cases or tears that impair knee function.
| Treatment | Description & Purpose | |
|---|---|---|
| Non-Surgical Management | ||
| Swelling & Pain Management | Rest, Ice, Compression, and Elevation (RICE) help reduce swelling and relieve pain in the early stages of injury. Pain medications and non-steroidal anti-inflammatory drugs (NSAIDs) may also be used to manage discomfort and inflammation. | |
| Supportive Bracing | Hinged knee braces or compression sleeves can provide stability, limit excessive movement, and reduce strain on the meniscus during healing. Unloader braces may also be used to shift pressure away from the injured area, improving comfort and mobility. | |
| Lifestyle Modification | Avoiding activities that strain the knee, such as deep squatting, twisting, high-impact sports, prolonged standing, and heavy lifting. Wearing supportive footwear and modifying movements can help protect the meniscus and promote recovery. | |
| Physiotherapy | A structured exercise programme strengthens surrounding muscles, improves knee stability, and restores function. | |
| Injection-Based Treatment | Includes corticosteroid injections to provide short-term relief by reducing inflammation and pain, hyaluronic acid injections to improve joint lubrication and help with early cartilage wear, and platelet-Rich Plasma (PRP) injections to promote healing and alleviate symptoms. | |
| Surgical Intervention | ||
| Arthroscopic Meniscus Repair | A minimally invasive procedure where a camera and specialised instruments are inserted to stitch back the torn. This is most suitable for younger individuals and tears near the outer edge, where improved blood flow supports healing after surgery. | |
| Partial / Total Meniscectomy | A partial meniscectomy trims the damaged portion of the meniscus to relieve symptoms and improve knee function, often for non-repairable tears. In severe cases, a total meniscectomy may be done to remove the entire meniscus, though it is generally avoided due to increased joint stress and osteoarthritis risk. | |
| Meniscus Transplant Surgery | In cases of severe meniscus loss, a meniscus transplant may be recommended, where a donor meniscus is surgically implanted to restore knee function and enhance joint stability. | |
Meniscus Tear Rehabilitation
The duration of rehabilitation for a meniscus tear depends on the severity of the
injury and the treatment approach.
Non-surgical recovery typically takes
4 to 6 weeks
with physiotherapy, while post-surgical rehabilitation can take 3 to 6
months,
focusing on progressive strengthening exercises to restore mobility and prevent re-injury.
Age, overall health, and adherence to rehabilitation protocols play a key role in recovery
speed and long-term knee function.
How to Prevent Meniscus Injuries?

While not all meniscus tears can be prevented, certain strategies can help reduce the risk:
- Strengthen knee-supporting muscles with targeted exercises.
- Wear appropriate footwear for sports and daily activities to improve stability.
- Avoid excessive squatting and sudden knee twists that place stress on the meniscus.
- Use proper lifting techniques to minimise strain on the knee joint.
Every patient deserves a treatment plan tailored to their needs. We start with non-surgical approaches before considering more invasive interventions.
Where Can I Find an Orthopaedic Surgeon for Meniscus Injury in Singapore?
Apex Novena
admin@apexsportsclinic.sg
101 Irrawaddy Rd, #18-12 Royal Square Medical Centre, Singapore 329565
Nearest MRT: NS20 Novena
Apex East Coast
admin@apexsportsclinic.sg
112 E Coast Rd, #03-03/04 i12 Katong, Singapore 428802
Nearest MRT: TE26 Marine Parade
Why Do Patients Choose Apex Sports Clinic?
Sports Doctor in Singapore: Personalised & Affordable Care
Progressive Treatment Philosophy
We prioritise personalised, non-invasive solutions, progressing to specialised treatments, including surgery, only when needed for more effective and targeted care.
Holistic Patient-Centred Care
From diagnosis to rehabilitation, we provide comprehensive and seamless care for a wide range of orthopaedic conditions.
Specialist in Sports Orthopaedics & Injury Management
We combine expert injury management with a proactive approach to maintaining your body's strength and function, so you can recover fully and perform at your peak.
Patient Journey
1 . Schedule Your Appointment

2 . Expert Diagnosis & Consultation

3 . Customised Treatment Plan

Schedule an Appointment

Our Insurance Partners






Frequently Asked Questions (FAQs)
A torn meniscus is a cartilage injury caused by twisting motions or forceful impact, often resulting in knee pain, swelling, and locking. Runner's knee, or patellofemoral pain syndrome, is an overuse injury due to muscle imbalances, improper knee tracking, or repetitive stress, typically causing pain around the kneecap. Consulting an orthopaedic specialist is recommended for a proper diagnosis through clinical assessment and imaging.
The best knee brace depends on the severity of the tear. Hinged braces provide stability for moderate to severe tears, while compression sleeves help reduce swelling in mild cases. It is advisable to consult an orthopaedic specialist or physiotherapist for a personalised recommendation.
A second meniscus tear can lead to increased knee instability, pain, and a higher risk of osteoarthritis. Treatment options may include physiotherapy, bracing, or surgery depending on the location and severity of the tear. It is best to consult your orthopaedic specialist to determine the most appropriate treatment approach.
Platelet-rich plasma (PRP) injections involve using a patient's own concentrated platelets to promote healing in the knee joint. While PRP may help with pain relief and inflammation, its effectiveness for meniscus tears is still debated. It is advisable to discuss with your doctor whether PRP is suitable for your condition.
A locked knee due to a meniscus tear feels as though the knee is stuck in one position, unable to fully straighten or bend. This is often caused by a large bucket-handle tear that physically obstructs knee movement. A locked knee typically indicates a more severe meniscus tear that may require surgical intervention. If you experience these symptoms, it is best to consult an orthopaedic specialist for proper evaluation and treatment.
Knee clicking from a meniscus tear may feel like a snapping or popping sensation when moving the knee. It is often accompanied by pain, swelling, or a feeling of the knee catching. Persistent clicking should be evaluated by a doctor or orthopaedic specialist.
Yes, in cases where most of the meniscus is severely damaged or removed, a meniscus transplant using a donor graft may be considered. This procedure is typically recommended for younger, active patients who do not have advanced arthritis, as the presence of significant arthritis reduces the success of the transplant. It is best to consult your orthopaedic specialist to determine if this option is suitable based on your knee condition.
Kinesio® tape can provide temporary support and reduce swelling, but it does not heal a meniscus tear. It may help alleviate mild discomfort during activity. It is advisable to consult your physiotherapist or doctor to ensure proper application and usage.
Externally, a torn meniscus may cause visible swelling around the knee joint but does not always produce noticeable changes on the skin. Symptoms such as pain, stiffness, difficulty bending or straightening your knee, and a sensation of locking or catching may indicate a torn meniscus. If you experience such symptoms, it is best to consult a doctor or orthopaedic specialist for proper diagnosis.
The medial meniscus is located on the inner side of the knee joint, between the thigh bone (femur) and shin bone (tibia). It helps distribute weight and absorb shock during movement.
The meniscus can be torn due to sudden twisting, pivoting, deep squatting, heavy lifting, or direct impact to the knee. Repetitive stress from sports, poor knee alignment, or weakened cartilage from aging can also contribute to degenerative tears over time.
The meniscus is located inside the knee joint between the femur and tibia, acting as a cushion to absorb shock and distribute weight. Each knee has two menisci: the medial (inner) and lateral (outer) meniscus.
The medial meniscus is located on the inner side of the knee and is more prone to injury due to its limited mobility and stronger attachment to surrounding structures. The lateral meniscus, found on the outer side, is more mobile and absorbs more rotational forces, making it less likely to tear.
The meniscus is composed of fibrocartilage, a strong yet flexible tissue that cushions the knee joint, absorbs shock, and enhances stability between the thigh bone (femur) and shin bone (tibia).
The medial meniscus is more prone to injury compared to the lateral meniscus because it is less mobile and more firmly attached to the knee joint structures. This makes it more susceptible to twisting forces and direct impacts, especially during sudden movements or high-impact activities.
A knee sprain involves stretched or torn ligaments, while a meniscus tear damages the cartilage cushioning the knee. Both cause pain and swelling, but a meniscus tear may also lead to locking or catching. If you have persistent knee discomfort, it is advisable to consult a doctor or orthopaedic specialist for a proper diagnosis.
While the meniscus itself cannot be directly strengthened, building the surrounding muscles helps support and protect the knee. Focus on quadriceps, hamstring, and calf exercises like leg presses, straight-leg raises, and hamstring curls. Low-impact activities like cycling and swimming can also improve stability. If you are unsure, it is best to consult a physiotherapist or orthopaedic specialist for tailored guidance.
Treatment depends on the severity of the tear. Mild cases may improve with rest, physiotherapy, and bracing, while severe tears may require surgical intervention such as meniscus repair or partial meniscectomy. It is best to consult a doctor or orthopaedic specialist who can determine the most appropriate course of treatment for your condition.
Common signs include knee pain, swelling, and a catching or locking sensation when moving the knee. If you experience such symptoms or have persistent knee discomfort, it is advisable to consult a doctor or orthopaedic specialist for proper diagnosis and treatment.
Walking may be okay or even beneficial for minor tears as it helps maintain joint mobility and blood circulation, which can aid recovery. However, it should be limited if it causes pain or worsens symptoms. It is best to follow your doctor or physiotherapist's advice on appropriate activity levels for your condition.
An untreated meniscus tear can worsen over time, leading to chronic pain, knee instability, and an increased risk of osteoarthritis. An untreated meniscus tear can worsen over time, leading to chronic pain, knee instability, and an increased risk of osteoarthritis. Early diagnosis and treatment can help prevent further damage and improve long-term knee function.
Non-surgical treatments include RICE therapy, pain management, physiotherapy, and knee bracing to reduce symptoms and support healing. Corticosteroid or PRP injections may also provide temporary relief. While mild tears may heal with these methods, larger tears may require medical intervention. It is best to consult an orthopaedic specialist to determine if surgery is necessary.
It is possible to walk with a torn meniscus, but pain, stiffness, and swelling may limit mobility. Walking should be done cautiously to avoid worsening the injury. It is best to follow your doctor's or physiotherapist's advice on managing movement and activity.
Low-impact exercises like straight-leg raises, seated knee extensions, and stationary cycling can help strengthen the knee while minimising strain on the meniscus. It is best to consult your doctor or physiotherapist for personalised recommendations on exercise and activity levels based on your condition.
Healing time depends on the severity of the tear and the chosen treatment. Minor tears may heal within 4 to 6 weeks, while recovery from surgery can take 3 to 6 months. Your orthopaedic specialist can provide a more detailed timeline based on your specific condition and treatment plan.
A knee brace can provide support and stability, particularly for moderate to severe tears. It is best to consult your doctor or physiotherapist if a knee brace is suitable for your recovery.
A doctor will conduct a physical examination, including tests like the McMurray test, to check for pain, clicking, or knee locking. An X-ray may be done to rule out bone injuries, while an MRI or ultrasound provides detailed imaging to confirm the meniscus tear and assess its severity.
Small, mild meniscus tears (Grade 1 or 2) may heal with rest, physiotherapy, and bracing, while severe tears (Grade 3) often require medical intervention. It is best to consult a specialist to determine the most appropriate treatment for your condition.
Ignoring a torn meniscus can lead to worsening pain, knee instability, and progressive cartilage deterioration, increasing the risk of osteoarthritis. Early diagnosis and treatment are crucial to preserving long-term knee function and preventing further joint damage.
Stationary cycling is often recommended as a low-impact exercise that strengthens the surrounding muscles while minimising strain on the knee. However, the suitability of cycling depends on the severity of the tear and individual recovery needs. It is best to consult your doctor or physiotherapist to determine if cycling is appropriate for your condition.
Meniscus tears in Singapore are treated with non-surgical options such as physiotherapy, pain management, and bracing, while severe cases may require surgical intervention like meniscus repair or partial meniscectomy. It is best to consult an orthopaedic specialist for a personalised treatment plan based on your condition.
Strengthening the knee, avoiding excessive twisting movements, wearing supportive footwear, and using proper techniques in sports can help prevent meniscus tears.
An untreated meniscus tear can worsen over time, leading to persistent pain, knee instability, and an increased risk of osteoarthritis due to ongoing cartilage damage. Early diagnosis and treatment are essential to prevent further deterioration and maintain long-term knee function.
Some mild meniscus tears can heal with physiotherapy, rest, and bracing, but more severe tears may require medical intervention such as injections or surgery. If you experience persistent pain or mobility issues, it is best to consult a doctor for an appropriate treatment plan.

