Cartilage Repair Singapore: Treatment Options & Care
Information reviewed by: Dr Foo Gen Lin | Last updated: Feb 20, 2026
Is cartilage damage causing joint pain or limiting your movement? Dr Foo provides personalised treatment options to address the damage and support long-term joint health.
MBBS (University of London) | MMed (Ortho) | FRCSEd (Ortho) | FAMS (Ortho)


What Is Cartilage Repair?
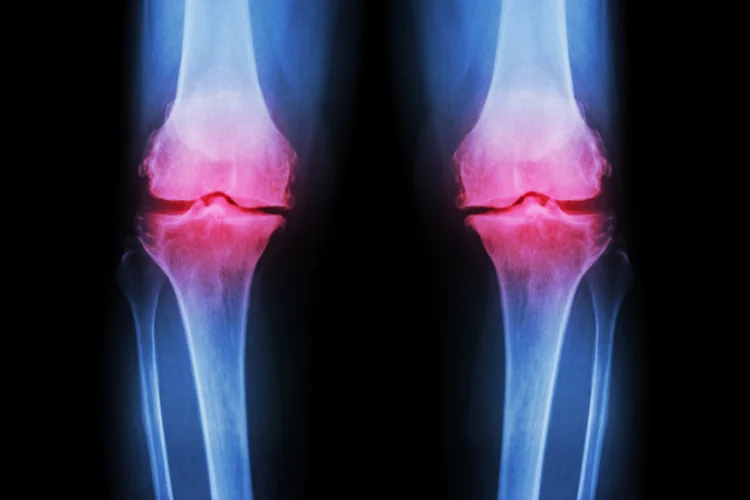
Cartilage repair refers to a range of medical procedures designed to address damaged
cartilage, the smooth tissue that cushions the ends of bones in joints and
allows them to move freely.
Cartilage can become damaged due to injury, repetitive stress,
or degenerative conditions such as osteoarthritis. This damage often results in pain,
stiffness, and reduced mobility in the affected joint.
Cartilage repair aims to restore joint function, reduce pain, and improve quality of life by
repairing or replacing the damaged cartilage with techniques tailored to the specific
condition.
Causes of Cartilage Damage
Cartilage damage can result from several factors, including trauma, ageing, and underlying medical conditions. Key contributors include:
- Ageing – As we age, cartilage naturally wears down, leading to thinning or degeneration.
- Physical Trauma – Sudden impact, excessive force, or abrupt twisting motions from sports, falls, or accidents can cause cartilage damage by creating shear stress, compression, or direct tearing within the joint.
- Repetitive Stress – Repeated movements or overuse of a joint can accelerate cartilage wear and tear.
- Obesity – Excess body weight places additional stress on weight-bearing joints like the knees, increasing the risk of cartilage damage.
- Poor Joint Alignment – Misaligned joints or altered biomechanics create uneven force distribution, increasing stress on specific areas of cartilage and leading to gradual deterioration over time.
- Medical Conditions – Conditions like arthritis (e.g., osteoarthritis, rheumatoid arthritis) and joint infections (such as septic arthritis) can accelerate cartilage breakdown and lead to long-term joint damage.
- Genetics – Inherited genetic variations can affect cartilage composition, repair capacity, and susceptibility to degeneration, increasing the risk of cartilage damage over time.
- Nutritional Deficiencies – Lack of essential nutrients, such as vitamin D, vitamin C, and minerals, can weaken cartilage, impair repair mechanisms, and increase susceptibility to degeneration.
Common Symptoms of Cartilage Damage

- Joint Pain – Pain often worsens with activity or after prolonged use of the joint.
- Stiffness – Reduced movement or flexibility in the affected joint, making it harder to fully extend or bend.
- Swelling – Inflammation or fluid build-up around the joint, causing visible puffiness.
- Popping or Clicking Sounds – These sounds can occur when the damaged cartilage causes uneven movement or rubbing in the joint.
How Is Cartilage Damage Diagnosed?
Diagnosing cartilage damage follows a structured evaluation process, starting with a medical history review, followed by a physical examination, imaging tests, and, if necessary, minimally invasive procedures to assess the cartilage directly.

- Medical History – Reviewing your symptoms, lifestyle, activity level, and any previous injuries or medical conditions that could contribute to cartilage damage.
- Physical Examination – Examining the affected joint for signs of swelling, stiffness, or abnormal movement, and performing specific manoeuvres to evaluate joint function.
- Imaging Tests – X-rays to help detect changes in bone structure and the presence of arthritis, while MRI scans provide detailed images of cartilage and soft tissue, allowing for a clearer assessment of the damage.
- Arthroscopy – In some cases, a minimally invasive procedure called arthroscopy may be used. This involves inserting a small camera into the joint to directly view the cartilage and determine the extent of the damage.
Types of Cartilage Repair Treatments
Treatment for cartilage damage focuses on relieving pain, improving joint function, and preventing further deterioration, with options varying based on the severity of the damage and the location of the injury. These treatments are generally categorised into non-surgical and surgical options:
| Treatment | Purpose |
|---|---|
| Non-Surgical Management | |
| Rest and Activity Modification | Limiting activities that strain the affected joint, such as high-impact exercises, helps reduce stress on the cartilage. Low-impact activities like swimming or cycling can be alternatives to maintain joint movement. |
| Physiotherapy | Tailored exercises strengthen the muscles surrounding the joint, providing better support and reducing stress on the cartilage. This also helps improve joint flexibility and range of motion. |
| Medication | Anti-inflammatory drugs or pain relievers may be prescribed to help control symptoms like pain and swelling. These medications provide temporary relief but do not address the underlying cartilage damage. |
| Injection-Based Treatment | These can include corticosteroid injections for inflammation and pain relief, hyaluronic acid injections to lubricate and improve joint function, and Platelet-Rich Plasma (PRP) therapy to stimulate healing and reduce inflammation. These options offer temporary relief but do not permanently repair cartilage damage. |
| Surgical Intervention | |
| Microfracture Surgery | This involves creating small holes in the underlying bone to stimulate the growth of new cartilage. It is particularly used for small to medium cartilage defects but may not work as well for larger areas of damage. |
| Autologous Chondrocyte Implantation (ACI) | A more advanced procedure where healthy cartilage cells are harvested from the patient, grown in a lab, and then re-implanted into the damaged area. This treatment is often used for larger cartilage defects, offering a long-term solution compared to traditional repair methods. |
| Osteochondral Allograft Transplantation | In cases of severe cartilage damage, this procedure involves transplanting healthy cartilage and bone from a donor to replace the damaged tissue in the joint. |
| Complete Joint Replacement | This procedure replaces the damaged joint (and cartilage) with a prosthetic, typically performed on joints like the knee, hip, or shoulder. It is considered for severe cartilage damage when other treatments are no longer effective, as it is a more invasive option. |
Recovery After Cartilage Repair
Recovery time depends on the type of treatment received. Non-surgical treatments typically offer a
quicker recovery, with many patients returning to normal activities within a few weeks.
However, surgical treatments may require several months for full recovery, often
involving physical therapy to restore joint function. It is essential to follow your doctor’s or
physiotherapist’s advice to ensure the best possible recovery.
Preventing Cartilage Damage
Preventing cartilage damage involves maintaining joint health and minimising risk factors. While some causes, such as ageing or genetics, are unavoidable, proactive measures can protect your joints:

- Maintain a Healthy Weight – Excess weight increases stress on weight-bearing joints, especially the knees and hips.
- Exercise Regularly – Low-impact activities like swimming, cycling, and walking keep joints active while minimising strain. Strengthening surrounding muscles provides better joint support.
- Practice Proper Posture and Joint Alignment – Good posture and correct movement mechanics help distribute forces evenly, reducing joint wear.
- Warm-Up and Cool Down – Prepares muscles and joints for movement while aiding recovery and injury prevention.
- Nutritional Support – A diet rich in vitamins, omega-3s, and glucosamine helps maintain cartilage, while hydration supports joint lubrication.
- Avoid Repetitive Strain – Take breaks and use proper techniques in activities involving repetitive motion to prevent overuse injuries.
Cartilage repair options range from non-surgical approaches to advanced surgical techniques. We assess each patient's situation to recommend the most appropriate path forward.
Find an Orthopaedic Specialist and Sports Doctor Near Me
Apex Novena
admin@apexsportsclinic.sg
101 Irrawaddy Rd, #18-12 Royal Square Medical Centre, Singapore 329565
Nearest MRT: NS20 Novena (3-min walk)
Wheelchair Accessible
Apex East Coast
admin@apexsportsclinic.sg
112 East Coast Rd, #03-03/04 i12 Katong, Singapore 428802
Nearest MRT: TE26 Marine Parade (7-min walk)
Wheelchair Accessible
Why Do Patients Choose Apex Sports Clinic?
Sports Doctor in Singapore: Personalised & Affordable Care
Progressive Treatment Philosophy
We prioritise personalised, non-invasive solutions, progressing to specialised treatments, including surgery, only when needed for more effective and targeted care.
Keyhole Surgery Expertise
We specialise in advanced arthroscopic keyhole surgery to treat sports injuries with precision and minimal tissue disruption, supporting faster recovery and restored joint function.
Specialist in Sports Orthopaedics & Injury Management
We combine expert injury management with a proactive approach to maintaining your body's strength and function, so you can recover fully and perform at your peak.
Patient Journey
1 . Schedule Your Appointment

2 . Expert Diagnosis & Consultation

3 . Customised Treatment Plan

Schedule an Appointment

Our Insurance Partners








Frequently Asked Questions (FAQs)
Glucosamine does not directly repair cartilage but may help slow cartilage breakdown and support joint health. It is a naturally occurring compound found in cartilage and is commonly taken as a supplement to reduce joint pain and stiffness, especially in osteoarthritis. While some studies suggest mild benefits in maintaining cartilage integrity, results remain mixed. If you're unsure, always consult your doctor before starting glucosamine or any joint supplement.
Knee cartilage has very limited ability to repair itself because it lacks blood supply, which is essential for healing. Minor cartilage injuries may improve with rest, physiotherapy, or supportive treatments, but larger defects usually require medical intervention such as injections or surgery. If you have persistent knee pain or swelling, it is advisable to consult a doctor or orthopaedic specialist for assessment and treatment options.
Foods rich in vitamins C and D, omega-3 fatty acids, collagen, and antioxidants can help support cartilage health. These nutrients aid collagen synthesis, reduce inflammation, and promote joint lubrication. Fatty fish, berries, citrus fruits, leafy greens, and bone broth are beneficial choices. While diet alone cannot reverse cartilage damage, balanced nutrition plays an important role in joint maintenance and recovery.
Yes, damaged cartilage can often be repaired or restored through non-surgical or surgical treatments depending on severity. Non-surgical methods such as physiotherapy, injections, and medication can help manage symptoms, while surgical options like microfracture or autologous chondrocyte implantation aim to regenerate new cartilage. If you suspect cartilage damage or experience symptoms, it is advisable to consult an orthopaedic specialist to determine the most appropriate treatment for your condition.
The success rate of cartilage repair varies depending on the procedure, patient age, and injury size. Microfracture surgery and cell-based therapies generally show good outcomes in improving pain and function, though results may decline over time. More advanced methods like autologous chondrocyte implantation can achieve longer-lasting results for larger defects. It is best to discuss expected outcomes and recovery timelines with your orthopaedic surgeon.
The cost of knee cartilage repair in Singapore varies widely based on the treatment type and severity of damage. Non-surgical options such as physiotherapy or injections may range from a few hundred dollars, while surgical procedures like microfracture, ACI, or graft transplantation can cost several thousand. Factors such as hospital fees, specialist expertise, and insurance coverage also affect total expenses. It is advisable to consult your orthopaedic specialist for an accurate estimate.
Knee cartilage surgery can be worthwhile for individuals with significant cartilage damage causing pain or mobility issues that do not respond to non-surgical treatments. It aims to restore joint function, relieve discomfort, and slow degeneration. The decision depends on factors such as age, activity level, and extent of injury. It is advisable to consult an orthopaedic specialist to determine whether surgical repair is appropriate for your condition and long-term goals.
Cartilage has limited capacity to regrow naturally, but non-surgical methods can support joint health and relieve symptoms. Physiotherapy, low-impact exercise, weight management, and injection-based treatments such as platelet-rich plasma (PRP) or hyaluronic acid may help maintain cartilage function and reduce inflammation. A nutrient-rich diet and proper joint care may also slow further damage. It is advisable to consult an orthopaedic specialist to explore suitable non-surgical options.
The most suitable treatment for damaged cartilage depends on the severity, location, and extent of the injury. Mild cases may respond to physiotherapy, medication, or joint injections, while more advanced damage may require surgical options such as microfracture or autologous chondrocyte implantation. Each method aims to reduce pain and restore joint function. If you suspect damaged cartilage or are experiencing symptoms, it is advisable to consult an orthopaedic specialist to determine the most appropriate treatment plan.
Common signs of cartilage damage include persistent joint pain, stiffness, swelling, and clicking or grinding sensations during movement. The affected joint may feel unstable or have reduced range of motion, particularly after activity or long periods of rest. These symptoms often worsen over time if untreated. If you experience ongoing discomfort or mobility issues, it is advisable to consult an orthopaedic specialist for proper evaluation and diagnosis.
Cartilage repair surgery typically takes between one and three hours, depending on the procedure and complexity of the defect. Minimally invasive techniques such as microfracture are usually shorter, while advanced procedures like autologous chondrocyte implantation or allograft transplantation may take longer. Recovery can take several months and often involves physiotherapy to restore strength and mobility. It is advisable to consult your doctor to understand the expected surgery duration and recovery timeline.
Many people can live with mild cartilage damage through symptom management and lifestyle modifications. However, untreated or progressive damage can lead to chronic pain, reduced mobility, and joint degeneration over time. Early diagnosis and appropriate treatment can help preserve joint function and quality of life. If pain or stiffness interferes with daily activities, it is advisable to consult an orthopaedic specialist for proper assessment and treatment.
Cartilage does not regrow in the same way as other tissues, but certain surgical techniques can stimulate the formation of new cartilage-like tissue. Procedures such as microfracture, autologous chondrocyte implantation, or graft transplantation aim to restore the joint surface and improve function. The new cartilage is often fibrocartilage, which is less durable than the original hyaline cartilage.
Knee cartilage surgery is performed under anaesthesia, so you will not feel pain during the procedure, though mild to moderate discomfort is common during recovery. Pain levels depend on the surgical method, extent of damage, and individual pain tolerance. Postoperative pain is typically managed with medication and physiotherapy. Most patients experience gradual improvement in pain and mobility as healing progresses. Always follow your surgeon's pain management and rehabilitation advice to ensure a smooth recovery.
Supplements such as glucosamine, chondroitin, collagen, and omega-3 fatty acids are commonly used to support joint and cartilage health. These nutrients may help reduce inflammation and maintain cartilage integrity but do not directly rebuild cartilage once it is damaged. Scientific evidence on their effectiveness varies. It is advisable to consult your doctor or specialist before starting any supplement to ensure it suits your medical condition and treatment plan.
Walking after cartilage surgery depends on the type and extent of the procedure. For minor repairs, limited weight-bearing with support may begin within days, while more extensive surgeries may require several weeks of restricted walking. Gradual physiotherapy-guided rehabilitation helps restore strength and mobility safely. Always follow your orthopaedic surgeon's and physiotherapist's instructions on when and how to resume walking after surgery.
Knee cartilage surgery carries risks such as infection, blood clots, joint stiffness, or incomplete cartilage healing. In some cases, pain or swelling may persist, and the regenerated cartilage may not match the durability of the original tissue. The risk level varies depending on the type of procedure and the patient's overall health. It is advisable to discuss potential complications and recovery expectations with your orthopaedic surgeon to determine whether the benefits outweigh the risks.
Collagen cannot directly rebuild cartilage, but it supports joint structure and may help slow cartilage degeneration. Collagen supplements are believed to stimulate cartilage-producing cells and improve joint elasticity, though scientific findings are mixed. A balanced diet rich in collagen-building nutrients, such as vitamin C and protein, can also promote joint health. It is advisable to consult your doctor or specialist before using collagen supplements for cartilage support.
Foods rich in omega-3 fatty acids, vitamins C and D, antioxidants, and collagen can support cartilage health and repair. Fatty fish, leafy greens, citrus fruits, berries, nuts, and bone broth are particularly beneficial. These nutrients help reduce inflammation, protect joint tissue, and promote collagen formation. While diet alone cannot reverse cartilage damage, it plays an important role in maintaining healthy joints and preventing further deterioration.

